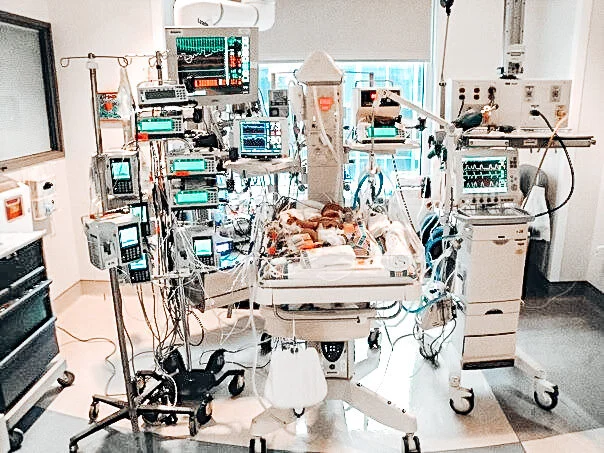
So, you are officially a new grad NICU RN. Congratulations, and welcome to the real worlD! You will soon learn that nursing school was a great foundation to teach you the importance of patient SAFETY, medical lingo, pharmacology, and of course the knowledge necessary to pass NCLEX! However, the reality of bedside nursing (especially the NICU) is very different from your nursing school experience. Here is a list of 40 tips I have compiled throughout the years to help with your transition into your new nursing role.
1. Never be afraid to ask questions.
Asking questions as a new grad can be very intimidating. For the safety of your babies, ALWAYS ASK. As they say, there are no stupid questions. Yes, there may be a lot that you know, but there is SO MUCH that you do not know. And it is very dangerous to have the “know it all” attitude as a brand new nurse.
2. Learn to admit your mistakes.
We all make them. Don’t make a habit of covering up a mistake, not reporting it, or trying to argue your way out of it. Your colleagues will understand if you own it and fess up. They will also help you so that it doesn’t happen again in the future. And if you do make one, don’t dwell on it. Learn from it and move on.
3. Always clarify if you have doubts.
Never hesitate to clarify an order, a medication indication, or a detail regarding your patient’s care if you are unsure about it. You may surprise yourself and catch something that a doctor overlooked!
4. Always safely check your bedside after your handoff report/shift change.
This includes IV assessment, suction, oxygen, code sheet, spare trach, alarm limits, bag & mask, IV fluids, etc.
5. Know the SIZES of all tubes and lines in your patient.
The NICU is a small and delicate population of patients. Attention to detail is vital. Examples of things to know: NG/OG tubes, IV gauge, PICC length out, chest tube, ETT, trach, UVC/UAC, foley catheter, etc.).
6. Keep up with your charting.
If you procrastinate and save it for later, there might not be enough time to complete it. Staying over to complete your charting is not fun. Remember that you cannot fully anticipate what the second half of your shift will look like. Prompt charting is important, but don’t compromise the quality and thoroughness over speed.
7. Don’t be too hard on yourself.
If you need to pee, go pee. Do not hold it in; it will just take a few minutes of your time. If you need to hydrate yourself, drink water before continuing with your tasks. Most nurses delay the little things they need because they focus on finishing a task, but in reality, if you are too hard on yourself, the work you do and your overall health can be affected.
8. Before calling a doctor, always think about and make an SBAR list of the things you need to communicate.
There is an old saying that we forget 80% of what we hear. Don’t trust your memory when calling a doctor, especially if he/she is in a hurry or tends to be intimidating. Relay your concern in a short, sweet, and straight-to-the-point manner so that the doctor can quickly understand your needs. And remember to read the order back and clarify.
9. Invest in your footwear and legwear.
You will walk a lot in your entire nursing career, so wear appropriate shoes that are made for ultimate comfort and durability. Clogs are notorious for being “ugly” but comfortable. They take about 2, 3, sometimes 4 weeks to completely break in, but the pricey investment is 100% worth it! And don’t forget those pesky compression stockings! Nursing involves a lot of footwork and prolonged standing. Take care of your legs early so you can avoid developing varicose veins.
10. Learn to be assertive.
This is something I am still working on daily. Learning your confidence takes time, but it’s important to stand your ground and SPEAK UP on behalf of your babies. You are serving as their advocate, being their voice, and communicating their needs.
11. Avoid being involved in workplace gossip.
It will do nothing good for your career as a nurse. Maintain professionalism and boundaries. If you have an issue with someone, talk to them directly and don’t let it escalate. If needed, though, you should follow your chain of commands to resolve the conflict.
12. Always look up your medications.
You are administering new medications that you don’t know. Take the time to understand dosage, compatibility, rate, indication, side effects, etc. And double check everything! Remember your 6 rights—patient, medication, dose, route, time, and documentation.
13. Read the doctors’ notes.
Oftentimes nurses forget to pass things along in their handoff report. Other times, information may not always be accurate. Make a habit of reading through the progress notes and plan of care before the end of your shift. You may find extra information you didn’t know or something that wasn’t mentioned.
14. Extend a helping hand to your colleagues when they need it.
You will soon realize how helpful it is to have caring coworkers. This also involves covering/picking up shifts for those in need. You’d be surprised at how your good deed can go a long way, especially when others are desperate. And oftentimes your peers will reciprocate the favor to show their gratitude.
15. When in DOUBT, take it OUT!
NICU IVs only usually last 24-96 hours depending on the baby’s vasculature. If it looks puffy, red, a little swollen, difficult to flush, or blanches, take it out. The last thing you want to be doing on your shift is administering Hyaluronidase (Wydase) for an IV extravasation/infiltration.
16. Don’t fully trust an IV pump or equipment.
Manually check the rate and volume (and concentrations) of the IV fluid during your rounds. Also, make sure that your pumps are plugged in. I can’t tell you how many times I’ve forgotten to check this. It’s shocking how quickly a battery charge on a computer, transport monitor, ventilator, medfusion pump, etc. lasts. You do not want to be in the middle of transporting your critical baby down to radiology and halfway there a vital piece of equipment starts alarming “low battery”!
17. When drawing up new medications or narcotics, always ask an experienced RN to watch you.
This will give you confidence and security knowing that you have prepared the right medication. Also ask how to reconstitute and administer the medication. And if you can’t find another nurse, phone a friend & call pharmacy! They are the experts! Because we give such small, diluted doses, it’s IMPERATIVE that you draw up your med correctly. 0.6mL of morphine is prepared completely differently than 0.06mL; if not done correctly it can cause respiratory depression and ultimately kill your baby!
18. Be careful with your charting.
Remember that if it’s not charted, it was NEVER done. Your charting will be very significant in case a lawsuit is brought against you or the hospital. If you didn’t document it, you didn’t do it!
19. Always appear calm and relaxed even if you are freaking out inside.
Parents notice everything and are always observing you. They watch your stress cues and will panic if you are panicking. A part of your job is calming down parents during times of crisis and emergency. It’s important to always maintain your composure.
20. Treat yourself at the end of a tiring, exhausting shift.
I like to reward myself after completing a long stretch of shifts (e.g. three in a row). This will give you the energy and motivation to continue and move forward. If you want that massive breakfast burrito, get it! If you want a glass (or bottle, no judgment) of wine after work, enjoy it! #TreatYoSelf
21. Be open to feedback and constructive criticism.
If a seasoned nurse suggests an easier way to do a task, try it. If your preceptor corrects you on a technique, thank them! Experience is the best teacher, and your senior nurses know it very well.
22. When you are working under a preceptor, this is the time to ask ALL the questions you have in your mind.
You are new and they know that. This is what your orientation process is designed for.
23. Time management.
Organize your shift and the tasks that you need to do. Writing them down on a piece of paper will help you to remember them. Use a “brain” or flowsheet. Prioritize what needs to be done first. You can also use it as a guide during shift report and charting.
24. Get to know everyone on your unit.
You don’t necessarily have to make friends with your peers outside of work, but getting to know your coworkers will help you adjust to your new environment and feel more comfortable asking for help. Immerse yourself in the culture of the unit while still maintaining professional boundaries with your colleagues.
25. Your first year as a nurse is the toughest.
All nurses who are new in the profession undergo the same period of adjustment, so be patient. You will have days that you feel incompetent and dumb. You will question yourself and your decision. You will drive home crying after a horrible day. You will contemplate calling in sick because of the fear and dread you have for your next shift. Don’t get in your own head. We’ve all been there. Trust yourself and push through the hard times because the end result is so worth it!
26. Avoid complaining.
Complaining at work affects the mood of your coworkers and makes you look ungrateful. Nobody wants a “negative Nancy” as a roommate or to be stuck in the same pod/zone as you for 12 hours. Try to stay positive and minimize negativity.
27. Delegate tasks.
You can’t do all of the work by yourself. It’s impossible even for nurses who have been on your unit forever. Delegate tasks to others within their scope of practice and in a respectful manner. And don’t be afraid to ask for help; nobody will look down upon you or think you’re inferior. In order to effectively time manage and stay on top of your cares, you must ask for help!
28. Develop your own support system.
It’s helpful to talk about your problems and struggles with someone who can understand what you’re going through. It can get very lonely if you don’t have anyone to confide in. Some hospitals even offer a mentor program, which would be a great resource to inquire about!
29. Set SMART goals for yourself.
Where do you see yourself in 5 years? Where do you want to be in 10? Setting career goals for yourself will help you to maximize your profession as a nurse and help you grow. In addition, communicating your aspirations and being transparent will help your manager/supervisor so that they can provide you with the tools necessary to help you get there.
30. Be flexible.
If you are asked to float to another unit for extra help, accept it. You will learn a lot from floating! Refer to my previous post about floating to hear why I recommend it! If you are asked to switch assignments, kindly oblige. If the oncoming nurse shows up late, call your husband and let him know you won’t make it home on time. $#!% happens. Roll with the punches and go with it.
31. When you’re faced with a crisis and you don’t know what to do, always start with the basics.
Obtain a full set of vital signs, perform your head to toe assessment, visualize and follow your lines, tubes, drains, etc. and examine your airway. The rest will stem from here.
32. Listen to your “gut feeling” and trust your instinct.
As you develop as a nurse, you will start to hone in on and recognize your nursing intuition. This is a feeling deep within you that should not be ignored. Research shows that our nursing intuition is simply more than a “gut feeling” but rather a validated component of nursing clinical care expertise. When we—as nurses—listen to our gut and speak up about our subjective feelings, the majority of the time we are correct. The strength of our intuition often urges us to do something more for our patients, and our experience enables us to recognize objective signs and symptoms unbeknownst to us. I encourage you to rely on your intuition and use this knowledge in clinical practice as a support in decision-making, which ultimately increases the quality and safety of patient care.
33. Leave your work at the hospital.
Go home with peace in your mind. It is unfair to think about what you might have forgotten to do at work when you are already at home with your family. I know it’s definitely easier said than done, though. I can’t tell you how many sleepless nights I’ve had, tossing and turning and wondering about the outcome of one of my babies. Nursing is a 24-hour job. There’s only so much you can do.
34. Leave your problems at the door.
The opposite is true for your personal life. Nothing in your private life should get in the way or interfere with your patient care. Sometimes, however, sharing a personal story with a grieving parent may help them to cope with their baby’s condition or an unfortunate circumstance. Unless you’re facing a major health crisis, I’m sorry to tell you this, but your coworkers probably do not care about what’s going on in your personal life.
35. If a doctor or more seasoned nurse grills you, don’t take it personally.
Remember that they know more than you, so take this as an opportunity to learn from them.
36. Do your physical assessment properly, as it will serve as the foundation of your care.
Practice it over and over with a systematic approach. Start with the head and work your way down. Soon, it will become second nature and you will do it in your sleep. Your examination should be speedy, accurate, and as detailed as possible.
37. Use proper body mechanics at all times.
When pushing equipment, lifting objects, moving isolettes, and even charting at your workstation, protect yourself by applying the principles of ergonomics.
38. Always disinfect at the beginning of your shift.
Remember that NICU babies are very vulnerable to acquiring infections. They have extremely weak, underdeveloped immune systems. After scrubbing in, wipe down “high-touch” surfaces such as bedside tables, stethoscopes, pumps, bottle warmers, doors, charts, chairs, etc. Everything that you plan on touching during your shift should be sanitized. Your cleaning does not take the place of EVS/housekeeping; it’s just an extra precaution.
39. Never forget the reason why you became a nurse.
Think about this reason whenever you are feeling tired, upset, disappointed, or burnt out from work. It will help you to get through the tough times of being a nurse.
40. Start your retirement early!
More than likely your organization provides a retirement plan. Start contributing to it NOW! This always seems to be put on the back burner; however, it should be one of the top things you prioritize for your future!