After huddle, report begins. A NICU report looks much different than the adult world and includes ALL (if not MOST) of the following, depending on your facility:
GENERAL
Baby’s name
Code status (Full, DNR, partial code, etc.)
Social history (CPS involvement, custody issues, etc.)
Any transmission precautions?
PREGNANCY AND DELIVERY
Age. Birth date + gestation, corrected gestational age, day of life.
Weight. Birth weight, current weight, gain or loss from the previous day.
Location of birth (hospital name, precipitous delivery in ER, homebirth, etc.).
APGAR scores.
Head circumference.
Length of the patient.
Events/complications during delivery (resuscitation measures needed + duration).
Primary diagnosis & reason for NICU admission.
MATERNAL HISTORY
Maternal age.
GTPAL.
Complications and health status (preeclampsia, IVF, etc.).
VITAL SIGNS
Temperature (36.5-37.5 C).
Heart rate (100-200).
Respiratory (10-100).
Blood pressure (MAP depends on age).
Apnea/Bradycardias/Desaturations.
Pain management (N-PASS).
GI/DIET
NPO, tube feeding or PO eating
Expressed breast milk, donor milk, or formula
Quality of oral feedings (nipple preference, pacing, timing, positioning, etc.).
Last BM (stool).
Abdominal girth.
Voiding type (diaper, ostomy, etc.).
Tube tube (OG, NG, Replogle, Anderson, or G tubes).
Tube purpose (decompression, feeding, intermittent/continuous suctioning).
Tube french size, length out, placement date (& when it’s due to be changed).
Last swallow study + results.
Last upper GI + results.
GU
Urine output (all diapers are weighed until discharge).
Foley (french size, reason for placement, date of placement, length out, & output).
IV ACCESS
Umbilical lines.
PICC line.
Peripheral IV.
TKO IV fluids
Broviac (sometimes).
TPN and Lipids.
D10W.
Any replacement fluids, such as albumin or sodium acetate?
RESPIRATORY SUPPORT
ETT size, placement on X-ray, number marked at gum, date of last intubation, date of last retape.
Ventilator type, mode, & settings (HFOV, SIMV, Bubble CPAP, Non-Invasive, HFNC, etc.).
Suctioning needs & characteristics of secretions.
FiO2 requirements.
Spell history, description, and management.
Last chest/abdominal X-ray + interpretation.
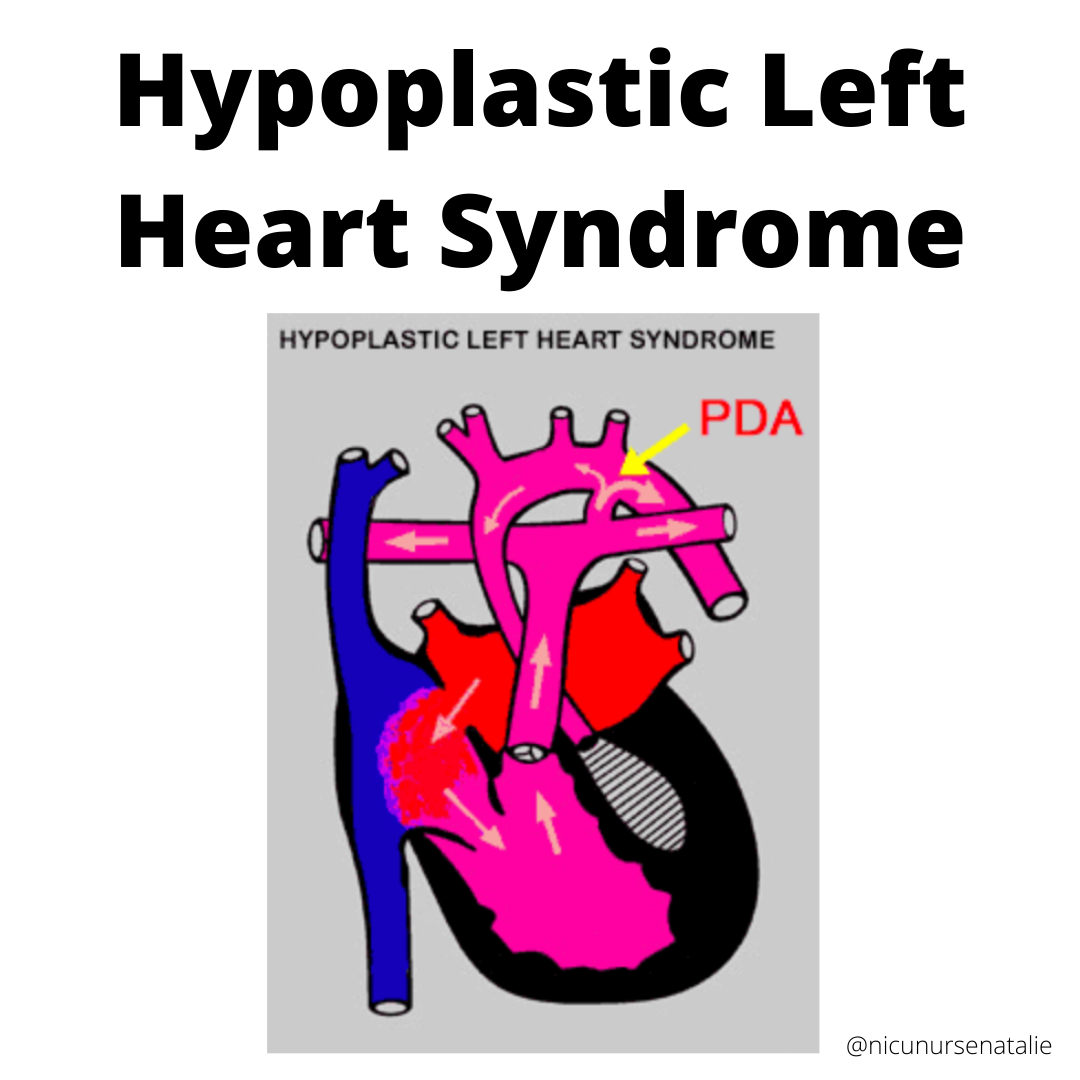
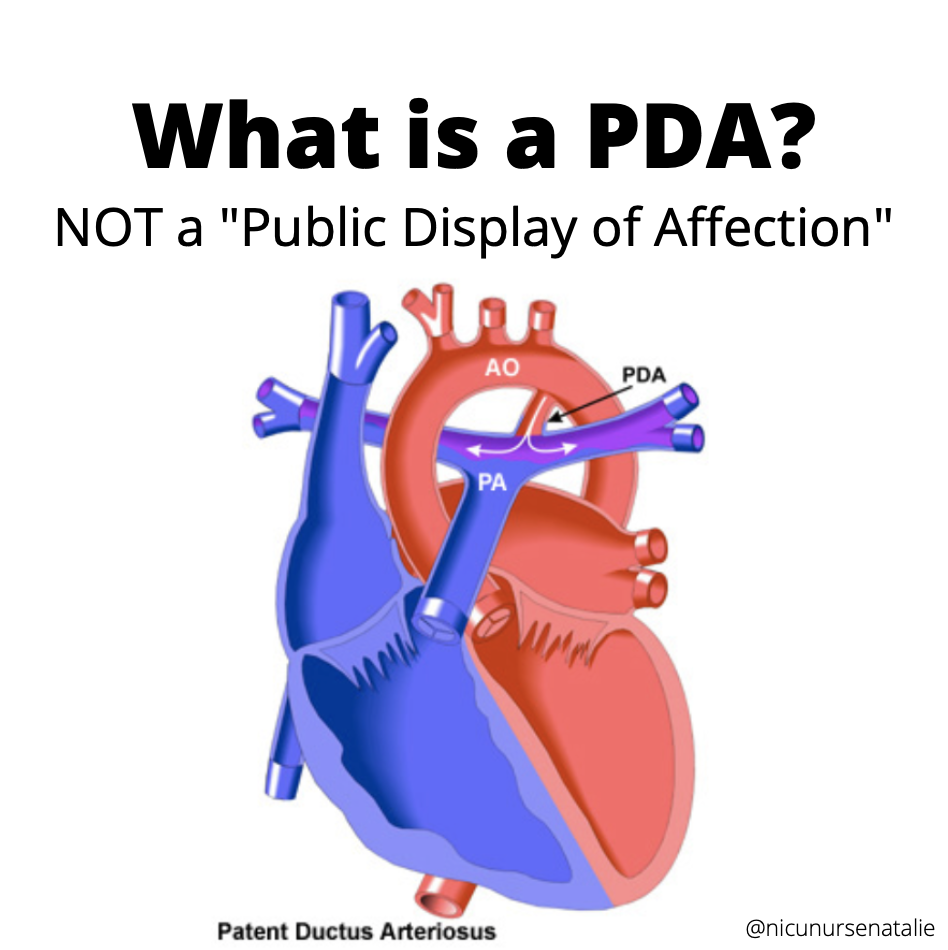
CARDIAC
Pulses (goal is +2).
Color (Pink, Pale, Mottled, Jaundice, etc.).
Cardiac meds (PGE, Dopa, Epi, Atropine etc.).
Last echocardiogram + interpretation.
NEURO
Tone of infant & neuromuscular status.
Last cerebral ultrasound (hydrocephalus, IVH, etc.).
Last MRI.
Last EEG.
Seizure history and management.
Last head circumference.
Neonatal Abstinence Scoring System scores over 24 hours.
INTEGUMENTARY
Last bath and products to use.
Skin tears, bruises, wounds.
LABS/HEMATOLOGY
Review lab trends (bilirubin, H|H, CMP, CRP, etc.).
CBGs.
Last blood transfusion.
OTHER DIAGNOSTICS
Last eye exam.
Last ultrasound (renal, abdominal, scrotal, etc.).
Last bone survey.
ORDERS:
Review all of the most recent lab results, shift medications, and look through all of the orders together.
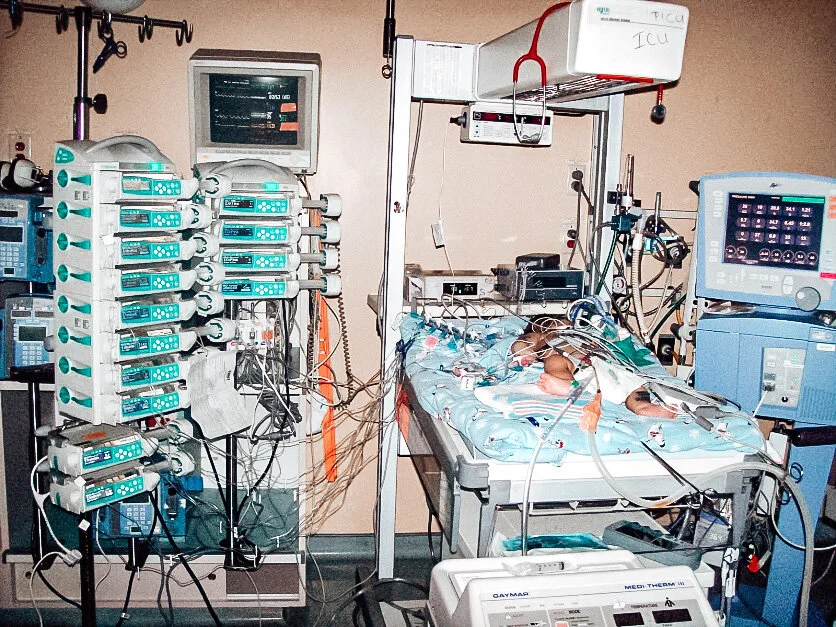
Lastly, walk to each of the babies’ bedsides (or just one bedside if you’re assigned a 1:1) together and look at everything. This includes double checking pumps, infusion rates, IV access, tube placement, settings, and connections.